Through our innovative and cutting-edge research, our world-class team has achieved scientific advances that no other group has accomplished, delivering new classes of therapeutics to treat patients with severe and life-threatening diseases and disorders. Let science lead the way
Omeros is advancing novel research and development programs for small-molecule and protein therapeutics to address both orphan and large-market indications. Our current areas of focus include complement-mediated diseases, central nervous system disorders and immuno-oncology. Tackling challenging diseases and disorders, we are targeting and exclusively control a broad range of previously untapped receptors and enzymes. The end result is first-in-class therapeutics designed to improve and save the lives of patients.
Research Areas
Complement-Mediated Disease
The complement system is an important part of the immune system and protects against invasive pathogens as well as damaged cells inside the body. When triggered, the various components of complement cooperate to generate an immune response that fights infection and clears damaged or dead cells, maintaining healthy function of the body’s systems. There are three distinct pathways of complement, each uniquely activated:
- Classical pathway: activated by antigen-antibody complexes
- Lectin pathway: activated by lectin binding of carbohydrate patterns on the surfaces of damaged cells and microbes
- Alternative pathway: constitutively active and amplifies classical and lectin pathway activation
Over- or under-activation (i.e., dysregulation) of this important system, however, can be harmful and is associated with increased vulnerability to infections and non-infectious diseases, including autoimmune disorders, chronic inflammation, thrombotic microangiopathy, and cancer. The involvement of the complement system in these and other diseases makes it a promising therapeutic target.
We are evaluating narsoplimab (OMS721) in lectin pathway-mediated diseases such as stem cell transplant-associated thrombotic microangiopathy (TA-TMA) and others.
Omeros is also studying OMS906 in a number of alternative pathway-mediated diseases including paroxysmal nocturnal hemoglobinuria (PNH), complement 3 glomerulopathy (C3G), and others.
Endothelial Injury Syndromes
Endothelial injury syndromes encompass a range of disorders associated with hematopoietic stem cell transplantation. Stem cell transplantation is used to treat a wide range of blood-related cancers, severe types of anemia and a variety of life-threatening immune disorders. Across all of these, the pretransplant chemotherapy regimens cause significant inflammation and endothelial damage. Then, as part of the stem cell transplant procedure, patients must undergo conditioning drug regimens followed by immunosuppressive therapy, each causing even more inflammation and endothelial damage. Components of endothelial injury syndrome associated with stem cell transplantation include thrombotic microangiopathy (TMA), veno-occlusive disease (VOD) and diffuse alveolar hemorrhage (DAH). Graft-versus-host disease (GvHD), a common complication of stem cell transplant, and infection also cause significant endothelial damage.
Hematopoietic Stem Cell Transplant-Associated Thrombotic Microangiopathy (TA-TMA)
Hematopoietic stem cell transplant-associated thrombotic microangiopathy (TA-TMA) is a significant and often lethal complication of stem cell transplants occurring in up to 39% of patients undergoing allogeneic HSCT1,2. This condition is a systemic, multifactorial disorder caused by endothelial cell damage induced by infection, GvHD, and marrow ablative agents used as part of stem cell transplantation. Activation of the complement system – primarily the lectin complement pathway – by endothelial damage plays a central role in the development of TA-TMA.
There are currently no approved products for the treatment or prevention of TA-TMA. We are developing narsoplimab, our antibody against MASP-2 (the effector enzyme of the lectin pathway), to treat TA-TMA.
1Postalcioglu M, Kim HT, Obut F, et al. Impact of thrombotic microangiopathy on renal outcomes and survival after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2018;24:2344-2353.
2Jodele S, Davies SM, Lane A, et al. Diagnostic and risk criteria for HSCT-associated thrombotic microangiopathy: A study in children and young adults. Blood. 2014;124:645-653.
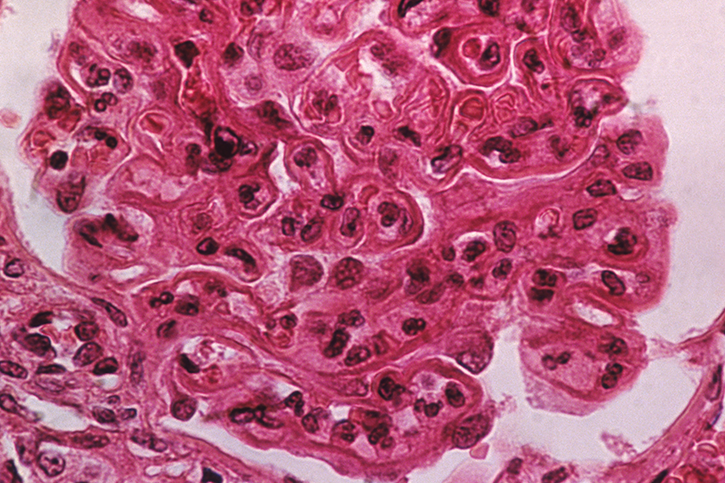
IgA Nephropathy
IgA nephropathy is the most common form of primary glomerulonephritis globally and is responsible for 10% of all dialysis patients worldwide. Up to 50% of IgA nephropathy patients develop end-stage renal disease and require dialysis within 20 years of diagnosis.1,2 Given the deleterious effects of steroids, there remains an unmet need for an alternative treatment option for IgA nephropathy.
1Hastings MC, Bursac Z, Julian BA, et al. Life Expectancy for Patients From the Southeastern United States With IgA Nephropathy. Kidney Int Rep. 2017;3(1):99-104.
2Schena FP. A retrospective analysis of the natural history of primary IgA nephropathy worldwide. Am J Med. 1990;89(2):209-215.
Lupus Nephritis
Lupus nephritis is an inflammatory kidney disease caused by systemic lupus erythematosus (SLE), an autoimmune disorder in which the body’s immune system attacks its own cells and organs. Kidney damage is common in SLE patients and may lead to kidney failure over time.
In a Phase 2 clinical trial, narsoplimab, our antibody against MASP-2 (the effector enzyme of the lectin pathway), reduced proteinuria by an unprecedented 70%. We plan to initiate a Phase 3 program for narsoplimab in lupus nephritis.
Paroxysmal nocturnal hemoglobinuria
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, life-threatening acquired disorder characterized by hemolytic anemia resulting from the absence of surface proteins (CD55 and CD59) that regulate hemolysis (i.e., red blood cell destruction) by the complement system. Left untreated, PNH is associated with debilitating anemia, a high risk of thrombosis, fatigue, and a severely reduced survival rate. Despite treatment with terminal complement inhibitors (i.e., C5 inhibitors), which inhibit intravascular but enhance extravascular hemolysis*, 63% of patients continue to experience hemolysis1, and approximately one third of them still require red blood cell transfusions2.
OMS906 is our lead antibody targeting MASP-3, the key activator of the alternative pathway. OMS906 is expected to block both intra- and extravascular hemolysis. Two open-label, multi-center clinical trials evaluating OMS906 in adult patients with PNH are ongoing.
*Extravascular hemolysis occurs when damaged red blood cells are removed by macrophages in the spleen or liver while intravascular hemolysis refers to cell destruction within blood vessels that releases free hemoglobin into plasma.
1Risitano AM et al. Blood. 2009;113(17):4094-4100.
2Kelly RJ, Hill A, Arnold LM, et al. Blood. 2011;117(25):6786-6792.
Leading Translational Research in Complement-Mediated Disease

In 2018, Omeros entered into a research collaboration with the University of Cambridge to establish the Omeros Center at Cambridge for Complement and Inflammation Research (OC3IR). One of the OC3IR’s priorities will be to characterize further the role of the complement system in endothelial injury, which is implicated in a wide range of diseases, including thrombotic microangiopathies and glomerulonephropathies. The Center will also facilitate collaborative links between Omeros and other leading academic research laboratories in the field of complement and inflammation research.
Central Nervous System Disorders
Addiction
One in six Americans 12 years of age or older experienced a substance use disorder in 20211, resulting in estimated societal costs in excess of several trillion dollars annually. Currently marketed drugs for addiction are, at best, only partially effective. Omeros discovered – and exclusively controls – the link between phosphodiesterase 7 (PDE7) and any form of addiction or compulsive disorder. We have shown that our PDE7 inhibitor OMS527 reduces both craving and relapse across animal models of nicotine, cocaine, opioid, and alcohol addiction as well as binge eating. PDE7 inhibitors also appear to avoid a major drawback of all currently marketed anti-addiction drugs – depression of the “reward system” or pleasure derived from other activities (e.g., social interaction, sex, sports, etc.), which is responsible for poor patient compliance. Importantly, PDE7 inhibitors have been shown to be nonaddictive in animal models.
1Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results From the 2021 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality. 2023.
Cocaine Use Disorder
Cocaine use disorder (CUD) is characterized by compulsive cocaine use despite adverse consequences. In the US, an estimated 1.4 million people have CUD and more than 24,000 people die each year from cocaine-related overdoses1,2. With no FDA-approved treatment, there remains a significant unmet need.
Cocaine inhibits the reuptake of dopamine and other monoamine neurotransmitters, eliciting dopamine surges – the primary mechanism through which cocaine evokes reward and initiates addiction. Chronic use of cocaine and other substances of abuse leads to dysregulation of dopamine transmission. PDE7 inhibition is thought to restore the physiological tone of dopamine transmission and counteract the negative effects of cocaine on the dopaminergic system.
The National Institute on Drug Abuse, part of the National Institutes of Health, has awarded Omeros a 3-year $6.69 million grant to support preclinical cocaine interaction studies and a randomized, single-dose, double-blind, parallel-group, inpatient study evaluating the safety and efficacy of OMS527 in patients with CUD*.
*Research described herein is supported by the National Institute on Drug Abuse of the National Institutes of Health under award number U01DA058541. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
1Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results From the 2021 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality. 2023.
2National Institute on Drug Abuse. Drug Overdose Death Rates. Updated February 9, 2023. Accessed March 22, 2023. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
Oncology
Our oncology programs are informed by a deep understanding of both the innate (complement-mediated) and adaptive (CD4 & CD8 T-cells) immune systems to derive highly differentiated, first-in-class therapeutic programs to treat a broad range of cancers.
While significant progress has been made within oncology through targeted therapies, advanced biologics (e.g., ADCs and RadioLigands), and immuno-therapies (e.g., checkpoint Inhibitors and CAR-T cellular therapies), Omeros is focused on moving beyond these approaches with a family of wholly novel cellular and molecular platforms. Driven by science, our discoveries have identified and evidenced the importance of certain molecules that selectively target T-cells to regulate a range of immune functions, including cancer suppression.
This has led to Omeros’ development of a new core therapeutic platform designed for broad application throughout oncology. The result is a portfolio of related programs comprising both signaling and antigen-driven immunomodulators, oncotoxins, immune memory-enhancing vaccines, and an adoptive T-cell technology that – unlike other cell therapy approaches – does not require cellular engineering.
Omeros’ in vitro and in vivo study data support the potential of our novel therapeutic platform to deliver effective and safe cancer therapies that can overcome the shortcomings of currently marketed therapies by:
- treating both hematological and solid tumors;
- targeting both cell-surface and intracellular cancer antigens; and
- increasing levels of CD4 and CD8 cancer antigen-specific effector and memory cells.
If successful, we believe that we will meaningfully change the cancer landscape for patients and for those who treat and care for them. Currently in stealth development, our oncology programs are advancing rapidly, and we expect to be in a position to share details about our oncology programs publicly within the coming months.
To learn more and start a conversation, please reach out at BD@Omeros.com
Related Pages